Community health centers (CHC) are critical in helping low-income and uninsured families live healthier lives and build strong communities. One in 15 people rely on CHCs for their comprehensive medical, oral, mental health, and substance abuse services, so it is easy to understand their impact.
Our mission is to deliver both the capital and commitment to foster facilities and innovations that increase access to health care services. We are the leading non-profit community health center lender in the country, and work with a variety of partners to create programs that improve health outcomes for those most in need.
Critical Safety Net
CHCs serve as the medical, dental, mental health, substance abuse, and special services lifeline for more than 22 million people nationally – a number that continues to rise each year. Especially in areas where access to quality care is limited, CHCs provide a valuable safety net.
Improving Access
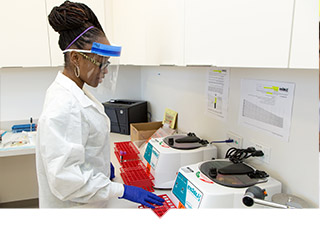
CHCs deliver quality care to low-income patients regardless of medical insurance or ability to pay. Focusing on equitable access to care, CHCs effect positive health outcomes for underserved communities who are otherwise priced out of the health care market.
Innovative Care
Studies show that CHCs’ focus on an ‘integrated care’ model improves quality of care, promotes better health and lower costs while creating thousands of jobs, spurring economic development. This focus on whole person well-being places the patient’s needs first.
OUR SOLUTIONS
Capital Impact Partners has three decades of practical experience working across the public, private and philanthropic sectors to create strategic financing and invest in the necessary infrastructure to increase access to high-quality health care and improve health outcomes through community health centers. In California alone, we are responsible for financing more than 50% of health centers and clinics across the state. We have also launched a national effort with AARP to help CHCs better serve our aging population.
Capacity Building
In partnership with The California Endowment and others, we are helping to expand the efforts of smaller health centers demonstrating innovative practices.
See our Capacity Building Efforts
Health Center Financing
Through our CPCA Ventures Loan Fund we provide health center loans for acquisition, construction, equipment purchasing and working capital from $1 million to more than $5 million, with ability to facilitate larger loans through special programs.
Review Our Financing Options
Convening Leaders
With support from policy makers, cities, and key partners, we bring industry leaders together to support policy change and spread innovative practices that support communities.
Learn about our Policy Work
Interested in applying for health center financing or partnering with us?
STORIES OF CHANGE
Our work happens across the country, but it’s the individual stories of change – how people’s lives are improved as their communities thrive – that fuel our mission. We serve those making change happen in big and small ways each and every day.
Unity Health Care
For many years, uninsured residents of Washington D.C.’s Ward 5 had to rely on a small, outdated clinic. That all changed when we helped Unity Health open a new 26,000 sq. ft. facility, vastly increasing its services offered to patients.
Tour the New Facility
South of Market Health Center
Providing a ‘private practice’ experience, this San Francisco clinic has engendered the pride of its many homeless and low-income patients who rely on these doctors for their only source of care.
Learn How South of Market Excels
Ole Health
OLE Health started as a humble clinic for farmworkers, but with our support, the health center now offers quality team-based care to all of Napa Valley’s vulnerable residents through their innovative integrated behavioral health model.
See Ole’s Team In Action
Brockton Neighborhood Health Center
With its origins as a mobile clinic, Brockton was looking to build a completely new facility in southern Massachusetts. This video demonstrates how Capital Impact (then operating at NCB Capital Impact) utilized a unique federal program to secure New Markets Tax Credit allocations and provide the financing Brockton needed. You’ll meet some of the staff and patients whose lives where changed for the better as a result of this $17 million health center as it vastly increased their capacity to serve the low-income, diverse, medically underserved patients in Brockton and surrounding communities.